Why Overachievers Never Get Sick 🧠
The Hidden Neuroscience of Stress, Immunity, and the "Let-Down Effect" (7min Read)
TL;DR – Why You Get Sick After Stress, Not During It
Your body temporarily boosts immunity under stress—but only so you can survive the moment.
Once the pressure lifts, your immune system crashes—that’s the Let-Down Effect.
Cortisol normally keeps inflammation in check… until your cells stop listening to it.
If you have CPTSD, this immune chaos isn’t just a phase—it’s your baseline.
Learn how trauma rewires your immunity and how to recover without burning out.
Why Do You Always Get Sick On Vacation?
Lemme ask you something: Have you ever gone on vacation and then all of a sudden started to get sick?
You’ve been crushing work for weeks without so much as a sneeze…
But the moment you finally rest, your throat gets sore, your head aches, and boom—you're sick.
You're not imagining it.
In fact, this strange timing of illness has a name in neuroscience and psychoneuroimmunology: The Let-Down Effect.
To really get it, we need to zoom in on the beautifully complex relationship between stress, your immune system, and your brain.
Today, we get to talk about all 3, and what you can do to prevent this from happening to you!
Let’s dive in.
Acute Stress: Your Body’s Emergency Defense Mode
Picture this: you’re being chased by a bear—or, more realistically, rushing to finish a big project with three minutes left on the clock.
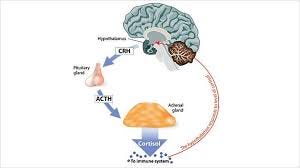
Your brain activates the hypothalamic-pituitary-adrenal (HPA) axis, unleashing stress hormones like cortisol and adrenaline.
These chemicals do more than just make you feel wired—they supercharge parts of your immune system:
Natural killer cells flood your system, prepping for injury or infection.
Inflammation ramps up slightly—just enough to offer extra defense.
Your immune cells get redistributed—mobilizing like first responders to the scene.
In the short term, this feels like a win.
You stay sharp, functional, and disease-free while you're in the trenches.
But this comes at a cost…
Cortisol: The Commander Who Can’t Be Ignored (Until It Is)
Cortisol doesn’t just flood your body during stress—it acts like a military general directing your immune troops.
In small doses, cortisol is incredibly helpful.
It tells your immune system where to go, what to do, and when to stand down.
It tempers inflammation, keeping it from becoming excessive or destructive.
This is why short bursts of stress can actually help you fight off invaders more efficiently.
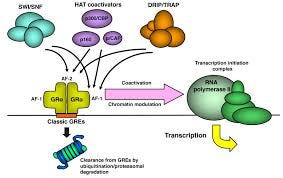
But if that general is always yelling orders—day after day, year after year—the troops eventually stop responding.
This is what scientists call “glucocorticoid receptor resistance,” which is a fancy way of saying that immune cells stop “listening” to cortisol’s instructions.
So, instead of calming things down, cortisol’s presence becomes noise, and inflammation runs unchecked, like a fire department ignoring a false alarm that turns out to be real.
Yikes… And we haven’t even gotten to chronic stress yet…
Chronic Stress: The Silent Saboteur of Immunity
If acute stress is a fire drill, chronic stress is living in a burning building.
Over time, the immune system can’t keep up with the demand.
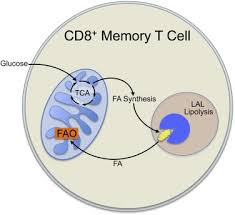
So your T-cell activity drops, making you more vulnerable to viruses.
Antibody production weakens, so you don’t fight off infections as well.
And immune cells stop “listening” to cortisol like we talked about above, leaving inflammation unchecked.
And yet—you don’t feel sick.
Why?
Stress-induced analgesia means pain signals are blunted.
Essentially, your body is numbing you to the signals…
Then, things like caffeine and the drive to achieve help you override fatigue.
All of which help you suppress inflammation and hide these symptoms—for now.
This is what makes anxious achievers so vulnerable.
You think you’re winning… until your body cashes in the bill and you crash.
Then Comes the Crash: The "Let-Down Effect"
You launched the product, you finished the product, and now it’s time for vacation.
You’re on the plane, fall asleep, and when you wake up, your throat gets a bit scratchy…
By the time you’re sitting beachside, your nose is running.
It’s right as you start to rest that it all hits you… Why?!
That's a great question, imaginary reader in my head, and it’s pretty simple to understand!
Cortisol drops suddenly, removing its anti-inflammatory control. Latent viruses like cold sores or mild infections can now flare.
Rebound immune activity leads to exaggerated inflammation. Headaches. Fatigue. Colds. Migraines.
Your pain sensitivity returns, revealing issues you couldn’t feel before.
This isn’t weakness—it’s biology.
It’s your body unmasking what it was protecting you from while you were “performing.”
Ok, but why Cody? I’m on vacation…
I get it, and I can summarize why in three words: Lions, Tigers & Bears
Why Your Body Falls Apart After the Stress Is Over: An Evolutionary Glitch
The Let-Down Effect might feel like your body betraying you—but it’s actually doing exactly what it was designed to do.
Back in the day, if you were running from a wild animal or fighting to survive, your body needed to keep it together until you were safe.
So it pumped out stress hormones like cortisol to supercharge your immune system—temporarily boosting defenses and blocking pain or illness until the crisis was over.
But here’s the catch: that high-alert mode wasn’t meant to last.
Once the danger passed, your body lowers cortisol levels, and the immune system relaxes.
That’s when injuries, infections, or exhaustion would finally show up—after you were safe.
Sound familiar?
Modern stress doesn’t come from lions or tigers—it comes from deadlines, unresolved trauma, burnout, and that never-ending to-do list.
But your body still plays by ancient rules.
It holds everything together while you're in survival mode, then lets go the second you slow down.
That’s the Let-Down Effect.
Not a failure, but a delayed reaction wired into your biology.
Think of it like a rubber band being stretched.
It holds tight under tension, but the second you release it—it snaps.
Psychoneuroimmunology: Where Mind, Brain, and Immune System Collide
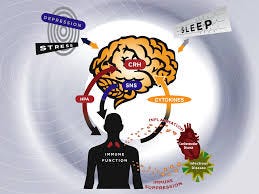
There’s a whole field of science that studies how your thoughts, nervous system, and immune system talk to each other.
It’s what I study, and it’s psychoneuroimmunology—and it helps explain exactly why you get sick when you finally rest.
Here’s how it works:
Stress starts in your brain.
When you're under pressure, your brain activates the HPA axis and your sympathetic nervous system—this is your body's fight-or-flight machinery.Your body releases stress hormones.
These include cortisol and adrenaline, which temporarily boost your immune system by increasing inflammation and mobilizing immune cells.But that boost comes at a price.
If stress continues, your immune system starts to shift gears:It lowers your production of antiviral cytokines (the ones that help fight off infections like colds and flu).
It increases pro-inflammatory cytokines, which can cause things like headaches, fatigue, joint pain, and brain fog.
Your immune system gets tired.
Over time, this stress-driven inflammation wears your immune system out. You lose the resources needed to mount a strong defense later on, especially after the stress ends.
Think of it like draining your phone battery during an emergency.
You keep using every last bit of energy to stay online, but once the crisis passes, your phone dies.
That’s your immune system on chronic stress: fully spent when you finally try to rest.
So when you stop pushing and your stress hormones drop, your immune system doesn't bounce back right away.
It’s already been running on empty.
That’s why symptoms show up after the stress ends—not during it.
What Happens When the Stress Never Ends?
For some of you though, the Let-Down Effect doesn’t quite fit.
You don’t only get sick after stress—you feel like your body is always struggling.
If that’s you, especially if you’ve lived through prolonged trauma, there’s a deeper layer at play.
People with Complex PTSD (CPTSD)—a trauma response rooted in long-term relational or developmental trauma—often live in a state of persistent physiological stress.
Unlike the temporary immune boosts seen in acute stress, CPTSD reshapes the immune system at a foundational level.
Chronic Inflammation as the Default
Pro-inflammatory cytokines remain elevated, not just during stressful moments but as a baseline, meaning you’re in a state of constant inflammation.
This is linked to autoimmune conditions and contributes to chronic fatigue, brain fog, and mood disorders.
Cortisol Confusion
In CPTSD, the HPA axis—your stress hormone command center—becomes dysregulated as well!
Your baseline cortisol levels are often low yet spike dramatically under stress.
Over time, immune cells become resistant to cortisol’s calming effect, leading to immune dysfunction and poor inflammation control.
Immune System Burnout
This burns out your immune system.
The body’s natural killer cells (first responders against viruses) are often suppressed.
T-cell activity and antibody responses decline, making people more vulnerable to infections—and even less responsive to vaccines.
Wounds, both physical and emotional, take longer to heal.
The Nervous System Stuck in Overdrive
And it’s not just your immune system; your nervous system is on high alert constantly, too!
The autonomic nervous system is locked in fight-or-flight mode.
It’s like the emergency brake is always on, which keeps the immune system in a confused, inefficient state—simultaneously inflamed and exhausted.
Yikes… Sadly, I see this all the time with my clients, and it comes at a cost.
CPTSD Health Fallout
This chronic immune dysregulation leads to:
Higher rates of autoimmune conditions
Frequent infections, even with “no obvious reason”
Neuroinflammation, contributing to cognitive fog and pain syndromes like fibromyalgia
Metabolic strain, increasing risks of cardiovascular disease and diabetes
If acute stress is a sprint that ends with collapse, CPTSD is like running a marathon with no finish line—and no shoes.
Understanding this helps explain why some people don’t just get sick after stress.
Their bodies have never stopped being stressed.
And that changes everything about how healing needs to happen.
Alright, Cody, I get it… What can I do about it?!
I’m glad you asked.
What You Can Do: 3 High-Impact Ways to Protect Your Body After Stress
Whether you’re someone who crashes only after the chaos ends—or someone living in a constant hum of stress—your body is doing its best to adapt.
But you can support it to recover better, regulate faster, and get sick less often.
Here are three evidence-backed strategies that work for both high achievers and trauma survivors!
1. Create a Gentle Landing After Stress (Don’t Just Crash)
Most people go from 100 to 0—slam through a deadline, then completely collapse.
That abrupt drop in cortisol is what triggers the Let-Down Effect.
Instead, try buffering the transition between stress and rest:
Schedule a lighter day after big deadlines or high-stress events.
Use low-stimulation downtime (walks, journaling, yoga nidra) before full rest.
For trauma survivors, this helps prevent dissociation or immune flare-ups when the system suddenly "lets go."
Think of it like cooling down after a sprint—you don’t just drop to the ground. You walk it out so your body catches up safely.
2. Do One Daily Practice That Actively Regulates Your Nervous System
You don’t need to meditate for 40 minutes.
But you do need a way to tell your body: "We’re safe now."
Choose one daily practice that downshifts your nervous system and recalibrates your HPA axis.
5–10 minutes of vagal stimulation: breathwork, humming, cold water face splashes.
IFS parts work, or gentle movements like restorative yoga or tai chi.
Even a long exhale breathing (inhale 4, exhale 8) done a few times a day can shift your immune signaling. I use a Komuso Shift to help me with this throughout the day.
Over time, these practices help restore cortisol rhythms and reduce chronic inflammation—making your immune system less likely to overreact or burn out.
3. Support Your Immune System Like It’s in Recovery—Because It Is
After a stress surge, your immune system needs to rebuild its reserves.
So, treat it like you would after an illness or injury!
Prioritize deep, consistent sleep—this is when immune repair happens.
Eat anti-inflammatory, immune-rebuilding foods (leafy greens, omega-3s, berries, mushrooms).
Cut back on caffeine and alcohol post-stress—they suppress immune repair and increase inflammation.
Yes, that means you should skip the mytai on the beach at first!
You’re Not Broken, You're Human
Remember, your immune system is like a dam holding back a flood.
When stress is high, the dam is reinforced to protect the town (your body).
But once the storm passes, the dam weakens—and all the built-up water rushes in.
This isn’t a failure of the dam—it’s just physics.
It's the same with your body.
So, if you’re someone who powers through pressure and collapses in calm—know that you're not broken.
You're biologically wired to protect yourself at all costs during stress.
But if you don't consciously help your body land after takeoff, the crash will come eventually.
You don’t need less drive—you just need better recovery.
And as always, until next time… Live Heroically! 🧠
Want to Work With Me? Here Are 3 Ways I Can Help You
Join the Balanced Creator Community (free): It’s the only community on earth built to support the mental health & mindset of content creators & entrepreneurs (creatorpreneurs) while growing and monetizing their brand and business.
Become a paid subscriber to the Mind, Brain, Body Lab Digest: You’ll get subscriber-only video posts, email replies, access to my entire blog archive, early access to new products, workshops & tools I create!
Work With Me 1on1 Through the Me 2.0 Program: Work with me 1on1 to heal the unresolved trauma and limiting beliefs that are holding back your health, wealth & relationships. (Extremely Limited Spots; Paid Subscribers Are Prioritized on Waitlist)
Supporting Research Section
Dhabhar, F. S. (2014). Effects of stress on immune function: the good, the bad, and the beautiful. Immunologic Research, 58(2–3), 193–210.
Segerstrom, S. C., & Miller, G. E. (2004). Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychological Bulletin, 130(4), 601–630.
Glaser, R., & Kiecolt-Glaser, J. K. (2005). Stress-induced immune dysfunction: implications for health. Nature Reviews Immunology, 5(3), 243–251.
Maier, S. F., & Watkins, L. R. (1998). Cytokines for psychologists: implications of bidirectional immune-to-brain communication for understanding behavior. Psychological Review, 105(1), 83–107.















This is a challenging read in terms of understanding the science, but it's so interesting and makes so much sense. I used to lecture in a prestigious sports college and all the staff would work flat out until the end of every term and then get sick...now I know why!